The coronavirus pandemic has transformed lives worldwide, bringing forth new challenges. While we grapple with these changes, a peculiar revelation emerges – COVID-19’s potential link to sleep issues. The pandemic’s ripple effect on mental and emotional well-being has been profound.
But is there a concrete relationship between COVID-19 and sleep disturbances? Let’s venture deeper into this connection.
COVID-19’s Direct Impact on Sleep

In the wake of COVID-19, various dimensions of our lives have experienced shifts, and one such dimension that hasn’t remained untouched is our resting. The virus has wielded an influence over our nightly rest, prompting us to wonder: what exactly about COVID-19 alters our sleep patterns?
Viral Factors
Viruses possess the intriguing capability to create ripples in our sleep patterns, a phenomenon linked to their interaction with neurotransmitters and brain structures intricately tied to the resting process.
As we delve into the realm of COVID-19, early-stage investigations suggest that this virus might exert comparable effects. These effects could potentially be attributed to the virus’s intricate relationship with the brain and the central nervous system, adding a layer of complexity to our understanding of its impacts.
Immune Response
The body’s formidable response to combat the virus introduces a new player into the arena: fatigue. This exhaustion, a frequent companion during illness, can be linked to the heightened immune activity required to vanquish the intruding virus.
Interestingly, this vigorous immune response occasionally interjects with our sleep cycle, causing it to become disrupted and resulting in nights of restless rest. It’s as if the body, while waging its battle against the virus, inadvertently throws a wrench into the delicate mechanics of our resting patterns.
Anxiety, Stress, and COVID-19
The COVID-19 pandemic, which swept across the globe, brought with it not just a health crisis but also a wave of emotional and psychological challenges.
One of the most profound impacts of the pandemic has been the surge in stress and anxiety levels among individuals, both of which have significant implications for sleep health.
Anxiety in the Context of the Pandemic:
Anxiety, by its very nature, is a state of heightened alertness and apprehension. During the pandemic, several factors have exacerbated this feeling:
Fear of the Unknown
The virus’s novel nature meant that there was a lot of uncertainty about its transmission, effects, and treatment. This uncertainty bred fear and anxiety in many.
Economic and Job Concerns
With businesses shutting down and economies taking a hit, concerns over job security and financial stability became paramount. For many, the fear of losing their livelihoods and the economic downturn added layers of anxiety.
Worry for Loved Ones

The contagious nature of the virus meant that everyone was at risk, leading to heightened concerns for the safety and well-being of family and friends, especially the elderly and those with underlying health conditions. When anxiety levels rise, the brain goes into an overactive mode, constantly processing threats and concerns.
This hyperactivity can make it challenging to relax and fall asleep, leading to prolonged periods of wakefulness and disrupted sleep patterns.
Stress and Its Impact on Resting:
Stress is the body’s natural response to challenging situations. However, chronic stress, like that experienced during the pandemic, can have detrimental effects on resting:
Cortisol and Sleep
Stress leads to the release of cortisol, often referred to as the “stress hormone.” Elevated cortisol levels, especially in the evening, can interfere with the body’s natural sleep-wake cycle. It can delay the onset of REM (Rapid Eye Movement) sleep, a critical phase of the resting cycle associated with dreaming and deep rest.
This disruption can result in fragmented sleep, frequent awakenings, and overall reduced rest quality.
The Vicious Cycle
An interesting yet concerning aspect of the stress-sleep relationship is its cyclical nature. A lack of restorative resting can make an individual more susceptible to stress, and increased stress can further disrupt sleep. This creates a feedback loop where one exacerbates the other, leading to a continuous cycle of poor rest and heightened stress.
Quarantine and Lifestyle Changes

The onset of lockdowns and the embrace of isolation ushered in more than just a pause in our usual routines; they orchestrated a profound transformation in the way we live each day, ultimately casting their influence over our circadian rhythms.
Routine Disruption: The pandemic-induced changes haven’t just altered our external environment; they’ve wielded an impact on our internal rhythm as well. The familiar markers of our daily lives – the predictable meal times, the bustling morning commute – have been reshuffled.
As a consequence, our internal clocks have been thrown off-kilter, prompting the emergence of irregular resting patterns. The steadiness that our routines once provided has been replaced by a sense of uncertainty, leading our sleep to mirror this sense of upheaval.
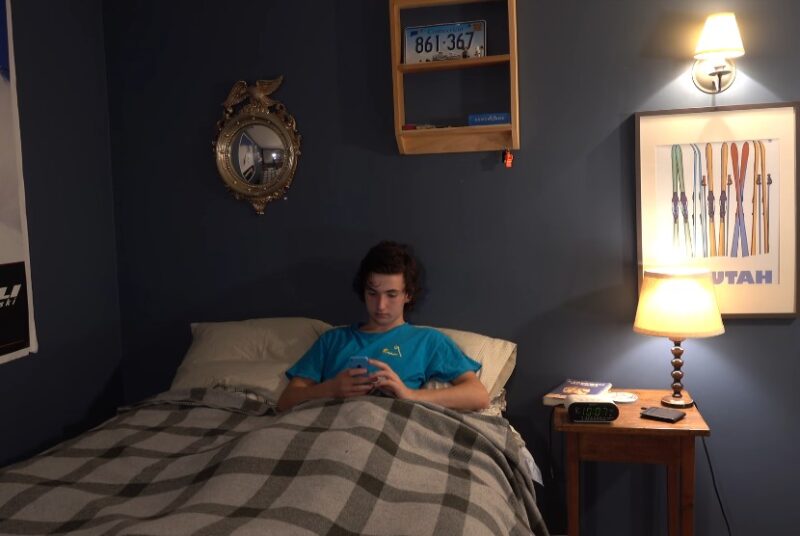
Overexposure to Screens:
Being confined indoors has increased our reliance on digital devices for work, entertainment, and social connection. The excess blue light exposure, especially during the evening, interferes with melatonin production, making resting elusive.
Long-Haulers and Chronic Symptoms
Some individuals, even after recovering from the acute phase of the virus, report lingering symptoms, among which resting disturbances feature prominently. These individuals, termed “long-haulers,” experience a range of symptoms, including dizziness, brain fog, fatigue, and sleep anomalies, extending weeks or even months beyond their initial recovery.
Why do These Issues Persist?
Ongoing research seeks to understand the persistent nature of these symptoms. Some theories suggest residual viral fragments or a prolonged inflammatory response as potential contributors to disrupted resting.
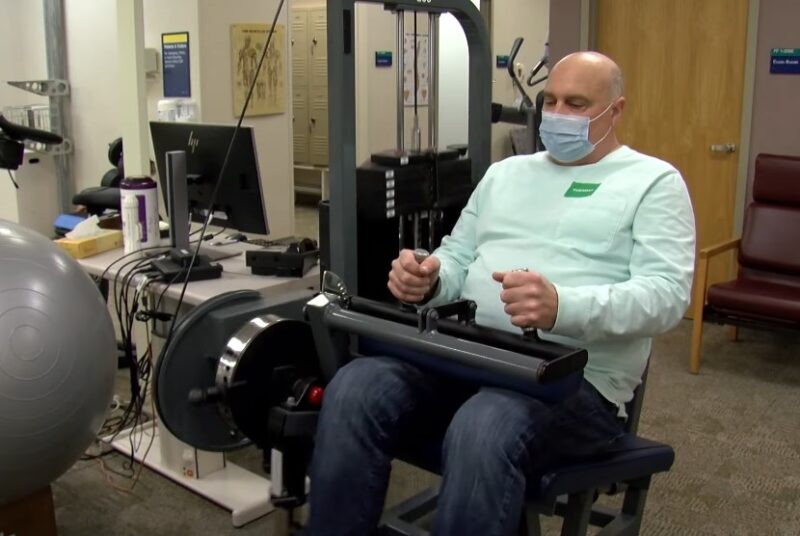
The Role of Respiratory Health
Given that COVID-19 targets the respiratory system, the implications for sleep, especially for those with pre-existing conditions, are significant.
Breathing and Resting:
Efficient respiratory function is essential for undisturbed sleep. Post-COVID respiratory complications can manifest as nocturnal breathlessness or frequent awakenings, further compromising resting quality.
Sleep Apnea Concerns:
Individuals with obstructive sleep apnea may experience worsened symptoms post-COVID, given the virus’s impact on respiratory muscles and lung function.
Mental Health and Isolation
The prolonged isolation and fear during the pandemic’s peak have escalated mental health challenges, intricately linked to resting quality.
Depression’s Influence:
With mental well-being on a decline for some, resting patterns are impacted. Depression can lead to both insomnia and hypersomnia, further highlighting the intertwined relationship.
Loneliness and Sleep:
Isolation can birth feelings of profound loneliness, a state associated with restless nights. The absence of regular social interactions can disrupt our body’s production of sleep-regulating neurotransmitters.
Moving Forward: Addressing Concerns

Acknowledging the profound relationship between COVID-19 and resting disruptions is the first step. But what proactive measures can individuals adopt? Incorporating practices such as a consistent bedtime, limiting caffeine and alcohol, and ensuring a dark and cool resting environment can enhance resting quality.
Seeking Professional Help:
Persistent issues should not be overlooked. Consulting specialists, and therapists, or even participating in cognitive-behavioral therapy for insomnia (CBT-I) can offer valuable solutions.
The Broader Implications
Beyond the individual, the societal ramifications of a sleep-deprived population during these times are considerable.
Economic Impact:
Sleep deprivation affects cognitive abilities, decision-making, and productivity. A community battling chronic issues could lead to diminished workplace productivity and, by extension, economic challenges.
Healthcare Strain:
With a rise in sleep-related concerns, healthcare systems might experience an influx of patients seeking treatments, placing an additional burden on already stretched resources.
Statistics Before the COVID-19 Pandemic
Before the emergence of the COVID-19 pandemic, the world was already witnessing a significant increase in sleep disturbances among individuals. Several factors contributed to this trend, and it’s essential to delve deeper into some of the primary reasons.
The Digital Age and Its Impact on Sleep:
We live in the digital age, an era marked by rapid technological advancements and an ever-increasing reliance on electronic devices. This period has brought about several lifestyle changes, including:
Extended Screen Time
With the proliferation of smartphones, tablets, and computers, people are spending more hours staring at screens than ever before. Whether it’s for work, entertainment, or socializing, screen time has become an integral part of our daily routines.
The blue light emitted from these devices can interfere with the production of melatonin, a hormone responsible for regulating resting. As a result, extended screen time, especially before bedtime, can lead to difficulty falling asleep.
Blurring Boundaries Between Work and Rest
The digital age has made it possible for many to work remotely, leading to flexible work hours. While this offers convenience, it also means that the lines between professional and personal time can become blurred.
It’s not uncommon for individuals to check work emails late at night or to continue working beyond traditional office hours. This encroachment of work into rest time can lead to increased stress and difficulty in switching off, both of which can adversely affect sleep quality.
Increased Exposure to Information
The constant influx of information, be it through news, social media, or other digital platforms, can be overwhelming. The brain remains active, processing this information, which can lead to overstimulation and difficulty in winding down at the end of the day.
FAQs:
How can one create a conducive environment for resting?
Reducing noise and light, using a quality mattress and pillow, and setting a comfortable room temperature can create a healthy setting.
When should one talk to a doctor about this problem?
If experiencing persistent symptoms of COVID-19, regular sleep difficulties, significant daytime sleepiness, episodes of waking up short of breath, loud snoring, or elevated levels of stress and mood changes.
What are the potential benefits of melatonin for COVID-19 patients?
Early-stage research suggests melatonin may improve resting quality in hospitalized COVID-19 patients and reduce the severity of the disease.
What is “long COVID”?
Long COVID describes symptoms that arise or persist one to three months after a COVID-19 infection.
How does COVID-19 affect the immune system in relation to sleep?
Resting is fundamental for a well-functioning immune system. Poor sleep may slow the body’s recovery from a coronavirus infection.
Conclusion: The Wake-Up Call!
Addressing sleep disturbances requires a unified approach, incorporating both individual efforts and policy-driven changes to support community well-being. With each passing day, new research offers insights into the virus’s far-reaching effects.
It’s essential to stay informed, adapt, and prioritize holistic health, with sleep at its core.
